Vaginitis
Most common causes of vaginitis:
Bacterial Vaginosis 22-50% (upper left image)
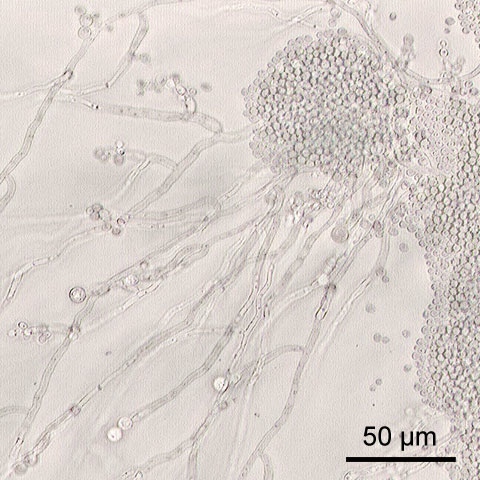
Vulvovaginal candidiasis 17-39% (lower right image)
Trichomoniasis 4-35% (upper right image)
Streptococcus - rare (lower left)
Images shared from Wikimedia Commons as Public Domain or through Creative Commons.
The background science:
Think of the vagina as an ecosystem. This is actually more than an analogy. Each person has what for them is a "normal flora". The organisms that compose this normal "flora" are many and comprise both bacteria and yeast. Some examples are lactobacillus, gardnerella, E. coli, group B strep and even candida. These various microbial populations of yeast and bacteria need to stay in reasonable balance. This makes for a healthy symptom free vagina. Once the ecosystem balance is disturbed for whatever reason, and symptoms develop, we say there is an infection.
Disturbing the ecosystem:
antibiotics
soap or cleansers to the perineum
douching
mechanical irritation or injury
poor immune function
abnormal blood sugars
foreign bodies
and more
Diagnosing vaginitis
Many of us think we can self diagnose or diagnose over the phone. Truth be told, many studies have shown that a reliable diagnosis cannot be made on basis of history alone. (2) Proper diagnosis requires a speculum exam, with pH test, and slide preparation for a microscopic exam. Yeast tends to produce an acid, or low pH, while BV produces a high, or more alkaline pH. The discharges for yeast can vary from clear to white or yellow, and have a sour yeasty odor, while the discharge for BV is foul or putrid smelling, and sometimes green or bloody. Because the vagina is such a complicated ecosystem in which sometimes some organisms are pathogenic and sometimes they are not, cultures per se are not helpful or diagnostic.
The upside of phone diagnosis is convenience. The downside is possible missed diagnosis, wasted money on inappropriate therapy and continued symptoms. In the case of untreated BV, there is risk of serious complications. Outside of pregnancy, this can mean deep pelvic infection, while in pregnancy it can mean miscarriage or early labor.
Treatments for yeast:
Over-the-counter anti-yeast medications - generally cheaper than prescription meds, but more often used incorrectly.
Prescription medications:
Terconazole- coming as cream or suppositories. Can be irritating initially.
Fluconazole - taken as a pill. May produce gastrointestinal symptoms.
The literature indicate theses two have comparable safety and effectiveness.
We teach our patients "The Three S's": No sweets, no soap, no sex, when a yeast infection is present.
We take yeast as an opportunity to counsel patients about their diet, exercise, and health habits in general, in the hopes that it will make the immune system more resilient.
Complicated yeast infections
We say yeast is complicated if it is recurrent, i.e. more than four times in a year, severe, resistant, or noted in a patient with diabetes or other serious medical conditions. Treatment in these cases is individualized. (3)
Treatments for Bacterial Vaginosis
First, it is important to realize that BV is caused by imbalances in different groups of bacteria. It is an abnormal preponderance of the anaerobic, or oxygen shunning bacteria. Treatment may be by tablets taken by mouth or creams or suppositories placed in the vagina. Medications include metronidazole and clindamycin. Treatment is critical for BV, since it may prevent miscarriage preterm labor, or serious pelvic infection.
Treatment for trichomonas, a swimming sexually transmitted organism, is with metronidazole or a related drug. Both patient and partner must be treated if trichomonas is present.
Metronidazole reacts with alcohol. Do not drink alcohol in any amount for three days before, during or after use of metronidazole. The reaction is violent nausea and vomiting.
Discuss all medications and their possible side effects in advance with your doctor.
Vaginal health problems are not something to ignore or tough out.
( 1 ), ( 2 ), ( 3 ) ACOG Practice Bulletin No. 72 Vaginitis